When the Doctor becomes the IVF Patient: an intro to my journey through fertility treatment
What medical school never taught me about being on the other side of reproductive medicine
The IVF Paradox: When the Doctor Becomes the Patient
There's something uniquely humbling about being a physician on the other side of fertility treatment. You'd think having an MD would give you a leg up in navigating the labyrinth of reproductive medicine. Instead, it mostly serves to illuminate how much we still don't understand about women's bodies, despite the eye-watering price tag and military-precision scheduling that comes with IVF.
The Physical Reality Check
Let's start with the FemVue (Hysterosalpingo-contrast sonography), shall we? There I was, a trained medical professional, reduced to a sweating, hand-crushing patient as bubbles illustrated my fallopian tubes. My partner's hand, trapped in my rigid little claw, served as collateral damage. It was a stark reminder that medical knowledge doesn't grant immunity from pain – and that we, as a profession, could do so much better with pain management in reproductive procedures. When Planned Parenthood announced sedation for IUD insertions, I nearly stood up and gave a standing ovation. Turns out, the cervix has opinions about being messed with, and maybe we should listen?
The Logistics Nightmare
The complexity of IVF would impress a NASA flight controller. Mixing medications with the precision of a compound pharmacist, timing injections like you're conducting a symphony, and showing up for monitoring appointments with the regularity of a Japanese train schedule.
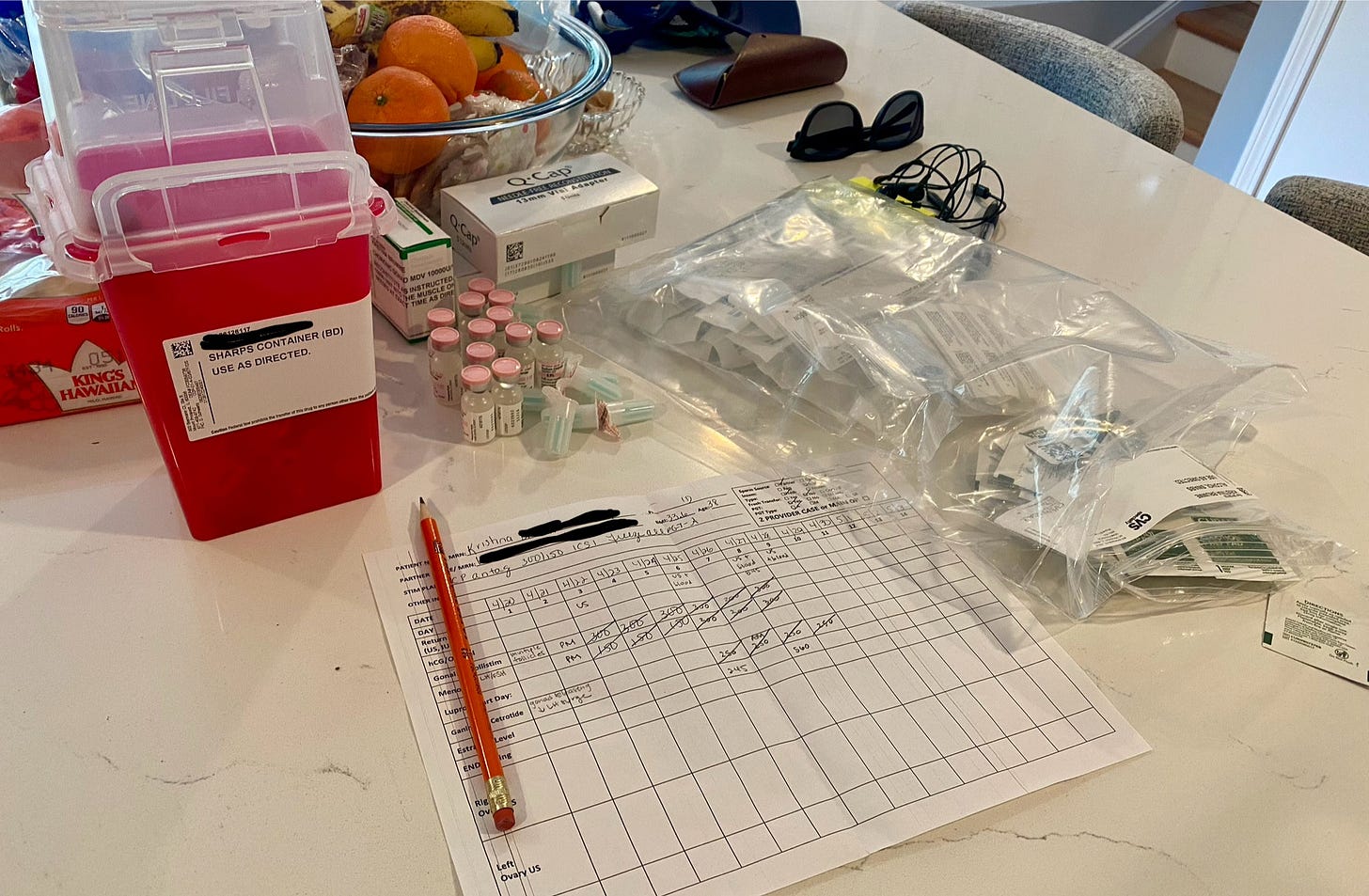
I had the "luxury" of working ten floors below my fertility clinic, and it was still a logistical circus. How do people manage this without proximity to their clinic? I've gained new respect for the stamina required to navigate this system.
Picture this: Half-dead after an overnight shift, apologizing to fertility clinic staff for my depleted veins while they played "find the blood vessel" – a game no one wants to win. Sure, I probably helped train some phlebotomists along the way, but at what cost to my already bruised arms? The awkward encounters with residents, colleagues, and high school acquaintances in the waiting room were just bonus entertainment.
This was further complicated when my partner unexpectedly had a permanent change of station to Sasebo, Japan and we had to make the necessary arrangements for…ahem…the materials for fertilization. Thankfully sperm retrieval is facilitated by a couple rooms that confusingly had not one, but three places to sit which gave us some a giggle about what a stool versus reclined position has to offer…
The Positivity Paradox
Can we talk about the relentless cheerleading that permeates fertility treatment? As someone who compulsively reads medical literature, I found myself craving evidence-based discussions instead of another round of "stay positive!" Cycle #1 was a total bonk - I could see in real time on ultrasound (mind you, I do ultrasound every day in the emergency department and I know my left ovary likes to hide) as one follicle that I referred to as the “bully follicle” out-competed the others like one giant tree finding sunlight and crushing all the little saplings below. Cycle #2 and 3 hit differently when all I wanted was hard data and realistic projections and to understand the why and the how of the adjustments.

Thank goodness for an REI physician friend who wasn't afraid to give it to me straight – discussing age-related statistics, protocol variations, and admitting when we're basically throwing darts at a board with some treatment decisions. Between her candid insights and diving into "IVF Hunger Games" data pulls (with an assist from AI for interpretation, more on this in a separate post), I finally felt like I was having the real conversations I needed. I’m impressed with the vulnerability of women sharing their stories which normalized the attrition and heartbreak when things “were going well” and the outcome isn’t what you wanted.

The Body Betrayal
Nothing in medical school prepared me for how IVF would feel in my own body. As someone whose stress manifests as nausea, I thought I knew what I was in for. Spoiler alert: I did not. The constant bloating made my follicles feel like they were floating in a jello mold. The nausea, the constipation, the whole hormonal symphony – it was like my body staging a revolution without consulting me first.
The cruel irony? Just when you need your usual stress relief the most, HIIT workouts become off-limits. My trusted endorphin source was replaced with gentle walks and a growing collection of stretchy pants. My joggers and slippers became my new best friends, while my workout gear gathered dust and judgment in the corner. And I know that it might seem like a diva complaint. Complaining about exercise over the possibility of reproducing? For a person who has had a lot of mental space tied up in the feeling of being in my body, I now could only feel like growth and maintenance of my body was being sacrificed. The upside, I know ALL the dogs in my neighborhood…
The Medical Disconnect
Perhaps the most jarring realization through this process has been confronting how limited our understanding truly is of reproductive medicine. For all our protocols and precise medication schedules, there's still so much that falls into the category of "well, this sometimes works and we're not entirely sure why." As a physician, this uncertainty is humbling. I handle this uncertainty in most of my conversations on shift. As a patient, it's terrifying.
The experience has left me with more questions than answers, both as a medical professional and as a patient. How can we better support patients through this process? Why aren't we investing more in research to understand the fundamentals of reproduction? And why, in 2025, are we still treating cervical procedures like they're no big deal?
For now, I'm learning to embrace the paradox of being both doctor and patient, of knowing too much and too little all at once. And maybe that's the biggest lesson here – that sometimes, even with all our medical knowledge, the best we can do is acknowledge our limitations and keep pushing for better understanding.
At least my joggers still fit.
If you need space to share details of your IVF journey, we are empathetic listeners, would love to hear about your biggest surprise through the process.
Disclaimer: The content provided in Couch Nap is for educational and entertainment purposes only. It is not intended as medical advice, diagnosis, or treatment. It does not establish a doctor-patient relationship. Always consult with your healthcare professional regarding any medical concerns or decisions. The views and opinions expressed here are our own and do not represent the positions, policies, or opinions of our employers or any affiliated organizations. While we strive for accuracy, the information presented here may not apply to your unique situation.